Candida (fungus)
This article is missing information about list of teleomorph genera e.g. Kluyveromyces; consider PMID 26526658 & PMID 33028600. (February 2022) |
| Candida | |
|---|---|
| |
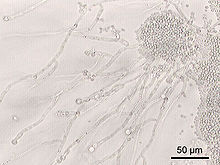
| Candida albicans at 200× magnification | |
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Saccharomycetaceae |
| Genus: | Candida Berkh. (1923) |
| Type species | |
| Candida vulgaris Berkh. (1923)
| |
Candida is a genus of yeasts. It is the most common cause of fungal infections worldwide and the largest genus of medically important yeasts.[1][2]
The genus Candida encompasses about 200 species.[2] Many species are harmless commensals or endosymbionts of hosts including humans. When mucosal barriers are disrupted or the immune system is compromised, however, they can invade and cause disease, known as an opportunistic infection.[3] Candida is located on most mucosal surfaces and mainly the gastrointestinal tract, along with the skin.[3] Candida albicans is one of the most commonly isolated species and can cause infections (candidiasis or thrush) in humans and other animals. In winemaking, some species of Candida can potentially spoil wines.[4]
Many species are found in gut flora, including C. albicans in mammalian hosts, whereas others live as endosymbionts in insects.[5][6][7] Systemic infections of the bloodstream and major organs (candidemia or invasive candidiasis), particularly in patients with an impaired immune system (immunocompromised), affect over 90,000 people a year in the US.[8]
The genome of several Candida species has been sequenced.[8]
Antibiotics promote yeast (fungal) infections, including gastrointestinal (GI) Candida overgrowth and penetration of the GI mucosa.[9] While women are more susceptible to genital yeast infections, men can also be infected. Certain factors, such as prolonged antibiotic use, increase the risk for both men and women. People with diabetes or the immunocompromised, such as those infected with HIV, are more susceptible to yeast infections.[10][11]
Candida antarctica and Candida rugosa are a source of industrially important lipases, while Candida krusei is prominently used to ferment cacao during chocolate production. Lipases from Candida rugosa are also used to digest fats in laboratory assays because of their broad range of activity.[12]
Biology
[edit]
When grown in a laboratory, Candida appears as large, round, white or cream (albicans means "whitish" in Latin) colonies, which emit a yeasty odor on agar plates at room temperature.[13] C. albicans ferments glucose and maltose to acid and gas, sucrose to acid, and does not ferment lactose, which helps to distinguish it from other Candida species.[14]
Recent molecular phylogenetic studies show that the genus Candida, as currently defined, is extremely polyphyletic (encompassing distantly-related species that do not form a natural group).[15] Before the advent of inexpensive molecular methods, yeasts that were isolated from infected patients were often called Candida without clear evidence of relationship to other Candida species. For example, Candida glabrata, Candida guilliermondii, and Candida lusitaniae are clearly misclassified[15] and will be placed in other genera once phylogenetic reorganization is complete (for example, see Khunnamwong et al. 2015).[16]
Some species of Candida use a non-standard genetic code in the translation of their nuclear genes into the amino acid sequences of polypeptides.[17] The difference in the genetic code between species possessing this alternative code is that the codon CUG (normally encoding the amino acid leucine) is translated by the yeast as a different amino acid, serine. The alternative translation of the CUG codon in these species is due to a novel nucleic acid sequence in the serine-tRNA (ser-tRNACAG), which has a guanosine located at position 33, 5' to the anticodon. In all other tRNAs, this position is normally occupied by a pyrimidine (often uridine). This genetic code change is the only such known alteration in cytoplasmic mRNA, in both the prokaryotes, and the eukaryotes, involving the reassignment of a sense codon.[18] This novel genetic code may be a mechanism for more rapid adaptation to the organism's environment, as well as playing an important role in the evolution of the genus Candida by creating genetic barriers that encouraged speciation.[18]
Pathogen
[edit]
Candida are almost universal in low numbers on healthy adult skin[14] and C. albicans is part of the normal flora of the mucous membranes of the respiratory, gastrointestinal and female genital tracts. The dryness of skin compared to other tissues prevents the growth of the fungus, but damaged skin or skin in intertriginous regions is more amenable to rapid growth.[19]
Overgrowth of several species, including C. albicans, can cause infections ranging from superficial, such as oropharyngeal candidiasis (thrush) or vulvovaginal candidiasis (vaginal candidiasis) and subpreputial candidiasis, which may cause balanitis, to systemic, such as fungemia and invasive candidiasis. Oral candidiasis is common in elderly denture-wearers.[20] In otherwise healthy individuals, these superficial infections can be cured with topical or systemic antifungal medications[21] (commonly over-the-counter antifungal treatments like miconazole or clotrimazole). In debilitated or immunocompromised patients, or if introduced intravenously (into the bloodstream), candidiasis may become a systemic disease producing abscesses, thrombophlebitis, endocarditis, or infections of the eyes or other organs.[8][14] Typically, relatively severe neutropenia (low neutrophils) is a prerequisite for Candida to pass through the defenses of the skin and cause disease in deeper tissues; in such cases, mechanical disruption of the infected skin sites is typically a factor in the fungal invasion of the deeper tissues.[19] The most common way to treat invasive candida infections is with the use of amphotericin or fluconazole; other methods would include surgery.[22]
Applications
[edit]C. albicans has been used in combination with carbon nanotubes (CNT) to produce stable electrically conductive bio-nano-composite tissue materials that have been used as temperature-sensing elements.[23]
Species
[edit]Among Candida species, C. albicans, which is a normal constituent of the human flora, a commensal of the skin and the gastrointestinal and genitourinary tracts, is responsible for the majority of Candida bloodstream infections (candidemia).[24] Yet, there is an increasing incidence of infections caused by C. glabrata and C. rugosa, which could be because they are frequently less susceptible to the currently used azole-group of antifungals.[25] Other medically important species include C. parapsilosis, C. tropicalis, C. dubliniensis.[8] and the more recently emerging pathogen C. auris.[26]
Other Candida species, such as C. oleophila, have been used as biological control agents in fruit.[27]
- C. albicans
- C. ascalaphidarum
- C. amphixiae
- C. antarctica
- C. argentea
- C. atlantica
- C. atmosphaerica
- C. auris
- C. blankii
- C. blattae
- C. boidinii
- C. bracarensis
- C. bromeliacearum
- C. carpophila
- C. carvajalis[28]
- C. catenulata
- C. cerambycidarum
- C. chauliodes
- C. corydali
- C. crusei
- C. dosseyi
- C. dubliniensis
- C. ergatensis
- C. fructus
- C. glabrata
- C. fermentati
- C. guilliermondii
- C. haemulonii
- C. humilis
- C. insectamens
- C. insectorum
- C. intermedia
- C. jeffresii
- C. kefyr
- C. keroseneae
- C. krusei
- C. lipolytica[29]
- C. lusitaniae
- C. lyxosophila
- C. maltosa
- C. marina
- C. membranifaciens
- C. mogii
- C. oleophila
- C. oregonensis
- C. parapsilosis
- C. quercitrusa
- C. rhizophoriensis
- C. rugosa
- C. sake
- C. sharkiensis
- C. shehatea
- C. temnochilae
- C. tenuis
- C. theae[30]
- C. tolerans
- C. tropicalis
- C. tsuchiyae
- C. sinolaborantium
- C. sojae
- C. subhashii
- C. viswanathii
- C. ubatubensis
- C. utilis
- C. zemplinina
References
[edit]- ^ Manolakaki, D.; Velmahos, G.; Kourkoumpetis, T.; Chang, Y.; Alam, H. B.; De Moya, M. M.; Mylonakis, E. (2010). "Candida infection and colonization among trauma patients". Virulence. 1 (5): 367–75. doi:10.4161/viru.1.5.12796. PMID 21178472.
- ^ a b Brandt, Mary E.; Lockhart, Shawn R. (2012-09-01). "Recent Taxonomic Developments with Candida and Other Opportunistic Yeasts". Current Fungal Infection Reports. 6 (3): 170–177. doi:10.1007/s12281-012-0094-x. ISSN 1936-377X. PMC 4626447. PMID 26526658. Archived from the original on 2024-02-23. Retrieved 2023-02-04.
- ^ a b Kourkoumpetis TK, Velmahos GC, Ziakas PD, Tampakakis E, Manolakaki D, Coleman JJ, Mylonakis E (2011). "The effect of cumulative length of hospital stay on the antifungal resistance of Candida strains isolated from critically ill surgical patients". Mycopathologia. 171 (2): 85–91. doi:10.1007/s11046-010-9369-3. PMC 4093797. PMID 20927595.
- ^ Fugelsang, K.; Edwards, C. (2010). Wine Microbiology (2nd ed.). Springer. pp. 3–28. ISBN 978-0387333496.
- ^ Spanakis EK, Kourkoumpetis TK, Livanis G, Peleg AY, Mylonakis E (2010). "Statin therapy and decreased incidence of positive Candida cultures among patients with type 2 diabetes mellitus undergoing gastrointestinal surgery". Mayo Clin. Proc. 85 (12): 1073–9. doi:10.4065/mcp.2010.0447. PMC 2996154. PMID 21123633.
- ^ Nguyen NH, Suh SO, Blackwell M (2007). "Five novel Candida species in insect-associated yeast clades isolated from Neuroptera and other insects". Mycologia. 99 (6): 842–858. doi:10.3852/mycologia.99.6.842. PMID 18333508.
- ^ Suh SO, Nguyen NH, Blackwell M (2008). "Yeasts isolated from plant-associated beetles and other insects: seven novel Candida species near Candida albicans". FEMS Yeast Res. 8 (1): 88–102. doi:10.1111/j.1567-1364.2007.00320.x. PMID 17986254.
- ^ a b c d d'Enfert, Christophe; Hube, Bernhard, eds. (2007). Candida: Comparative and Functional Genomics. Caister Academic Press. ISBN 978-1-904455-13-4.
- ^ Kennedy MJ, Volz PA, Edwards CA, Yancey RJ (1987). "Mechanisms of association of Candida albicans with intestinal mucosa". J. Med. Microbiol. 24 (4): 333–41. doi:10.1099/00222615-24-4-333. PMID 3320372.
- ^ Steckelberg, James M. (2012-09-18). "Male yeast infection: Can I get it from my girlfriend?". Mayo Clinic. Archived from the original on 2023-06-07. Retrieved 2014-03-23.
- ^ "Yeast Infections". MedlinePlus. Archived from the original on 2014-04-01. Retrieved 2014-03-23.
- ^ Menden, Ariane; Hall, Davane; Paris, Daniel; Mathura, Venkatarian; Crawford, Fiona; Mullan, Michael; Crynen, Stefan; Ait-Ghezala, Ghania (15 August 2019). "A fast, miniaturised in-vitro assay developed for quantification of lipase enzyme activity". Journal of Enzyme Inhibition and Medicinal Chemistry. 34 (1): 1474–1480. doi:10.1080/14756366.2019.1651312. PMC 6713963. PMID 31414611.
- ^ "Candida species". DoctorFungus.org. Archived from the original on 2007-02-08. Retrieved 2007-02-09.
- ^ a b c Meyers, Frederick H.; Jawetz, Ernest; Goldfien, Alan (1978). Review of Medical Pharmacology (6th ed.). Lange Medical Publications. ISBN 978-0-87041-151-9.
- ^ a b Fitzpatrick, David A; Logue, Mary E; Stajich, Jason E; Butler, Geraldine (2006). "A fungal phylogeny based on 42 complete genomes derived from supertree and combined gene analysis". BMC Evolutionary Biology. 6: 99. doi:10.1186/1471-2148-6-99. PMC 1679813. PMID 17121679.
- ^ Khunnamwong P, Lertwattanasakul N, Jindamorakot S, Limtong S, Lachance MA (2015). "Description of Diutina gen. nov., Diutina siamensis, f.a. sp. nov., and reassignment of Candida catenulata, Candida mesorugosa, Candida neorugosa, Candida pseudorugosa, Candida ranongensis, Candida rugosa and Candida scorzettiae to the genus Diutina". International Journal of Systematic and Evolutionary Microbiology. 65 (12): 4701–9. doi:10.1099/ijsem.0.000634. PMID 26410375.
- ^ "CGD Help: Non-standard Genetic Codes". Candida Genome Database. Archived from the original on 1 November 2018. Retrieved 1 May 2015.
- ^ a b Santos, Manuel A. S.; Ueda, Takuya; Watanabe, Kimitsuna; Tuite, Mick F. (31 October 2003). "The non-standard genetic code of Candida spp.: an evolving genetic code or a novel mechanism for adaptation?". Molecular Microbiology. 26 (3): 423–431. doi:10.1046/j.1365-2958.1997.5891961.x. PMID 9402014. S2CID 13575999.
- ^ a b Goehring, Richard V. (2008). Mims' Medical Microbiology (4th ed.). Philadelphia, Pennsylvania: Mosby Elsevier. p. 656. ISBN 9780323044752.
- ^ Darwazeh A, Lamey P, Samaranayake L, MacFarlane T, Fisher B, Macrury S, MacCuish A (1990). "The relationship between colonisation, secretor status and in-vitro adhesion of Candida albicans to buccal epithelial cells from diabetics". Journal of Medical Microbiology. 33 (1): 43–49. doi:10.1099/00222615-33-1-43. PMID 2231671.
- ^ "Yeast Infections (Candidiasis) in Men and Women". WebMD. 2012-11-12. Archived from the original on 2012-08-19. Retrieved 2014-03-23.
- ^ Gamaletsou, Maria N.; Rammaert, Blandine; Bueno, Marimelle A.; Sipsas, Nikolaos V.; Moriyama, Brad; Kontoyiannis, Dimitrios P.; Roilides, Emmanuel; Zeller, Valerie; Taj-Aldeen, Saad J. (January 2016). "Candida Arthritis: Analysis of 112 Pediatric and Adult Cases". Open Forum Infectious Diseases. 3 (1): ofv207. doi:10.1093/ofid/ofv207. ISSN 2328-8957. PMC 4742637. PMID 26858961.
- ^ Di Giacomo, R (2013-03-07). "Candida albicans/MWCNTs: A Stable Conductive Bio-Nanocomposite and Its Temperature-Sensing Properties". IEEE Transactions on Nanotechnology. 12 (2): 111–114. Bibcode:2013ITNan..12..111D. doi:10.1109/TNANO.2013.2239308. ISSN 1536-125X. S2CID 26949825.
- ^ Gow, Neil A. R.; Yadav, Bhawna (2017). "Microbe Profile: Candida albicans: a shape-changing, opportunistic pathogenic fungus of humans". Microbiology. 163 (8): 1145–1147. doi:10.1099/mic.0.000499. hdl:2164/12360. PMID 28809155.
- ^ Pfaller, M. A.; Diekema, D. J.; Colombo, A. L.; Kibbler, C.; Ng, K. P.; Gibbs, D. L.; Newell, V. A. (2006). "Candida rugosa, an emerging fungal pathogen with resistance to azoles: geographic and temporal trends from the ARTEMIS DISK antifungal surveillance program". Journal of Clinical Microbiology. 44 (10): 3578–3582. doi:10.1128/JCM.00863-06. PMC 1594768. PMID 17021085.
- ^ Spivak, Emily S.; Hanson, Kimberly E. (2017). "Candida auris: an Emerging Fungal Pathogen". Journal of Clinical Microbiology. 56 (2). doi:10.1128/JCM.01588-17. PMC 5786713. PMID 29167291.
- ^ "Efficacy of Candida oleophila strain 128 in preventing Penicillium Expansum infection in apricot fruit". Acta Horticulturae. 485: 141–148. 1999. Archived from the original on 2018-11-06. Retrieved 2006-11-17.
- ^ James, S. A.; Carvajal Barriga, E. J.; Bond, C. J.; Cross, K.; Núñez, N. C.; Portero, P. B.; Roberts, I. N. (2009). "Candida carvajalissp. Nov., an ascomycetous yeast species from the Ecuadorian Amazon jungle". FEMS Yeast Research. 9 (5): 784–788. doi:10.1111/j.1567-1364.2009.00518.x. PMID 19459983.
- ^ Simonetti, Omar; Zerbato, Verena; Sincovich, Sara; Cosimi, Lavinia; Zorat, Francesca; Costantino, Venera; Di Santolo, Manuela; Busetti, Marina; Di Bella, Stefano; Principe, Luigi; Luzzati, Roberto (2023-04-01). "Candida lipolytica Bloodstream Infection in an Adult Patient with COVID-19 and Alcohol Use Disorder: A Unique Case and a Systematic Review of the Literature". Antibiotics. 12 (4): 691. doi:10.3390/antibiotics12040691. ISSN 2079-6382. PMC 10135169. PMID 37107053.
- ^ Chang, C. F.; Lin, Y. C.; Chen, S. F.; Carvajal Barriga, E. J.; Barahona, P. P.; James, S. A.; Bond, C. J.; Roberts, I. N.; Lee, C. F. (2012). "Candida theae sp. nov., a new anamorphic beverage-associated member of the Lodderomyces clade". International Journal of Food Microbiology. 153 (1–2): 10–14. doi:10.1016/j.ijfoodmicro.2011.09.012. PMID 22088606.
External links
[edit]- Labs working on Candida
 The dictionary definition of Candida at Wiktionary
The dictionary definition of Candida at Wiktionary
